For many medical professionals, the decision to open a private practice is both aspirational and practical. It represents a shift from working under the administrative policies of hospitals or group practices to creating an environment tailored to their own professional values and patient care philosophies. However, the transition from employee to owner carries with it a significant shift in responsibility. Physicians must weigh whether they are driven by self-direction, financial incentive, or a desire for more personalized patient relationships.
Before taking the leap, it is important to analyze whether one’s personality and skills align with the demands of ownership. Running a practice requires a willingness to manage people, budgets, and operations in addition to providing medical care. Medical expertise alone is not sufficient; practitioners must be prepared to make executive decisions and embrace the entrepreneurial side of medicine. A comprehensive self-assessment can help gauge readiness for the complexities that come with ownership.
Additionally, physicians should reflect on the long-term commitment involved. Owning a practice is not just a career move but a lifestyle choice. The hours can be long, and the burdens of ownership can feel constant. A deep understanding of what motivates the decision will help provide the resilience needed to sustain the practice through challenges and change.
Table of Contents
Navigating Legal and Regulatory Requirements
One of the most critical early steps in launching a medical practice is ensuring compliance with the law. The healthcare industry is among the most heavily regulated, with federal, state, and local laws all playing a role in shaping operations. Licensing requirements, malpractice insurance, HIPAA regulations, and professional liability protections must all be accounted for before opening the doors to patients. Failure to comply with legal standards can lead to significant fines and even revocation of a medical license.
Physicians must also choose the correct business structure for their practice, which impacts taxes, liability, and future growth potential. Whether forming a sole proprietorship, a partnership, or a professional corporation, each has distinct advantages and obligations. Legal counsel should be retained to draft key documents, such as operating agreements and employment contracts. These documents must reflect not just the current needs but also anticipate future developments, such as adding partners or expanding services.
During this phase, many physicians find value in partnering with platforms like Collaborating Docs, which offer practical insights into various subjects such as practice setup, development, and operations. Whether it’s guidance on business structures, compliance, or day-to-day logistics, exploring strategies tailored to the healthcare space can help streamline decision-making. Attention to these behind-the-scenes aspects of practice setup, such as credentialing processes, regulatory filings, and operational planning, can reduce the risk of early complications. Aligning clinical goals with practical business execution is what ultimately lays the foundation for a resilient and compliant practice.
Securing Financing and Budgeting Wisely
Opening a medical practice requires a substantial financial investment. From purchasing or leasing office space to acquiring medical equipment, the costs can easily exceed initial estimates. Physicians must develop a detailed business plan that includes projected revenues, overhead costs, and startup capital needs. Without a clear financial roadmap, the likelihood of overextending financially increases significantly.
Securing financing can be one of the more challenging aspects for new practitioners. Traditional lenders may require a solid credit history, collateral, or even prior business experience. In many cases, specialized healthcare lenders can offer more tailored options that align with the unique needs of medical startups. Regardless of the source, physicians should approach borrowing with caution and ensure they fully understand the terms, including repayment schedules and interest rates.
It is also essential to budget for the unexpected. Emergency repairs, fluctuating patient volume, or delays in insurance reimbursements can place strain on finances. Building a cash reserve and factoring in contingency planning will help ensure operational stability during the first crucial years. A well-structured budget is not just a financial tool but a blueprint for long-term sustainability.
Choosing the Right Location and Facility
Location plays a pivotal role in the success of a medical practice. The ideal site is accessible, visible, and aligned with the demographics of the target patient population. Physicians must conduct thorough market research to identify underserved areas or communities where demand for their specialty is high. Factors such as parking availability, public transportation access, and neighborhood safety also play into patients’ decision to seek care.
In addition to choosing the geographic location, selecting the right type of facility is equally important. A modern, welcoming office with adequate space for patient care, administration, and future expansion contributes to both patient satisfaction and staff efficiency. The design should comply with ADA requirements, infection control standards, and state health department regulations. Even small design choices, such as waiting room layout or lighting, can significantly affect the patient experience.
Lease agreements or property purchases should be reviewed carefully to ensure favorable terms. Hidden fees, maintenance responsibilities, and restrictions on modifications can become costly surprises if not identified upfront. Engaging a commercial real estate agent with healthcare industry experience can help physicians avoid common pitfalls and secure a location that supports long-term growth.
Building an Effective Administrative Infrastructure
Running a medical practice is as much about business administration as it is about clinical care. Physicians must invest in creating a back-office infrastructure that supports scheduling, billing, insurance claims, compliance, and communication. This includes selecting the right electronic health record (EHR) system, hiring qualified administrative staff, and establishing workflows that promote accuracy and efficiency.
One of the biggest operational challenges new practices face is billing and revenue cycle management. Mistakes in coding or delays in claim submission can result in lost income or audits. Whether handled in-house or outsourced, billing operations must be handled by experienced professionals. Physicians should also track key performance indicators such as claim rejection rates, days in accounts receivable, and patient no-show rates to ensure financial health.
Additionally, a well-run administrative system contributes to patient satisfaction. Efficient scheduling, responsive communication, and transparent billing all play a role in how patients perceive the quality of care. Investing in technology that automates routine tasks and improves the patient interface can give a new practice a competitive advantage in today’s increasingly consumer-driven healthcare environment.
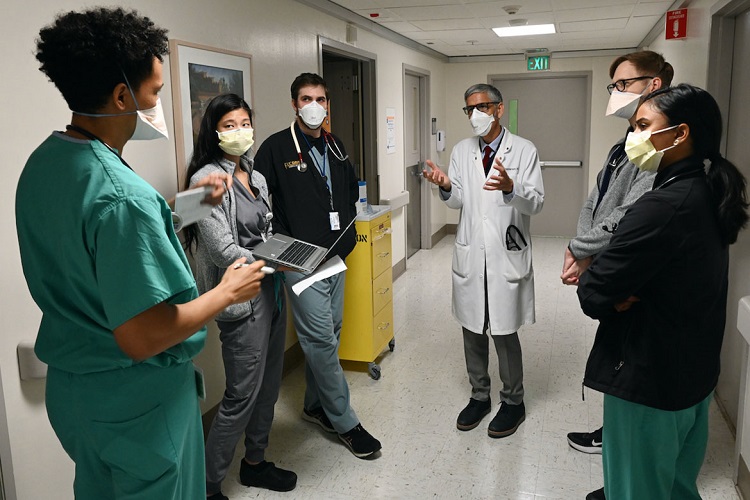
Hiring and Managing a Strong Team
The quality of staff can make or break a medical practice. From front-desk receptionists to clinical support staff, each team member contributes to the overall patient experience. Physicians must be deliberate in hiring, seeking individuals who are not only competent but also align with the practice’s values and culture. The interview process should evaluate both technical proficiency and interpersonal skills, as patient engagement is a critical component of healthcare delivery.
Beyond hiring, effective team management is essential. Physicians must take on leadership roles, providing clear expectations, training, and feedback. Employee retention often depends on creating a workplace where staff feel respected, supported, and empowered. Regular performance evaluations, professional development opportunities, and a positive workplace culture contribute to long-term team stability.
Moreover, legal and regulatory considerations extend to human resources as well. Practices must comply with labor laws, including wage standards, workplace safety, and anti-discrimination regulations. Employment contracts and job descriptions should be carefully written to avoid legal ambiguity. A strong HR foundation helps minimize risk and supports sustainable growth.
Developing a Marketing and Patient Acquisition Strategy
In today’s competitive healthcare market, simply opening a practice is not enough. Physicians must actively market their services to attract and retain patients. This involves creating a professional brand, establishing an online presence, and leveraging digital marketing tools such as search engine optimization (SEO), pay-per-click advertising, and patient reviews. Building a reputation takes time, but early outreach can accelerate growth.
Physicians should also engage in community-based marketing efforts. Partnering with local organizations, participating in health fairs, or offering free educational seminars can establish the practice as a trusted community resource. Word-of-mouth referrals remain a powerful tool, and satisfied patients often become advocates for the practice. Building these grassroots connections is particularly important for specialists or those entering saturated markets.
Tracking the effectiveness of marketing strategies is crucial. Analytics tools can provide insight into website traffic, ad performance, and patient demographics. By regularly reviewing this data, physicians can adjust their marketing efforts for greater impact. A consistent, patient-focused message that highlights the practice’s unique value proposition will help differentiate it in a crowded field.
Planning for Long-Term Growth and Succession
Opening a practice is only the beginning. For long-term success, physicians must plan for the future. This means setting strategic goals for growth, such as expanding services, opening additional locations, or hiring more providers. These goals should be supported by measurable milestones and a realistic timeline. Periodic reviews of the business plan can ensure the practice remains aligned with its evolving vision.
Succession planning is another critical but often overlooked aspect. Whether the plan is to retire, sell the practice, or bring in a partner, having a strategy in place ensures continuity of care for patients and financial security for the physician. Succession plans should include legal documents, transition timelines, and mechanisms for valuing the practice. Early planning allows for a smoother transition and protects the legacy of the practice.
Finally, professional development should continue throughout the life of the practice. Staying current with clinical guidelines, emerging technologies, and industry trends helps maintain excellence in patient care. Participating in peer networks or business forums can also provide valuable insight and support. A growth mindset ensures that the practice not only survives but thrives in the ever-changing landscape of healthcare.